Insulin-like growth factor 1
Insulin-like growth factor 1 (IGF-1), also called somatomedin C, is a hormone similar in molecular structure to insulin which plays an important role in childhood growth, and has anabolic effects in adults.[5] In the 1950s IGF-1 was called "sulfation factor" because it stimulated sulfation of cartilage in vitro,[6] and in the 1970s due to its effects it was termed "nonsuppressible insulin-like activity" (NSILA).[7]
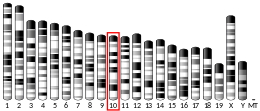
IGF-1 is a protein that in humans is encoded by the IGF1 gene.[8][9] IGF-1 consists of 70 amino acids in a single chain with three intramolecular disulfide bridges. IGF-1 has a molecular weight of 7,649 daltons.[10] In dogs, an ancient mutation in IGF1 is the primary cause of the toy phenotype.[11]
IGF-1 is produced primarily by the liver. Production is stimulated by growth hormone (GH). Most of IGF-1 is bound to one of 6 binding proteins (IGF-BP). IGFBP-1 is regulated by insulin. IGF-1 is produced throughout life; the highest rates of IGF-1 production occur during the pubertal growth spurt.[12] The lowest levels occur in infancy and old age.[13][14]
A synthetic analog of IGF-1, mecasermin, is used for the treatment of growth failure in children with severe IGF-1 deficiency.[15] Cyclic glycine-proline (cGP) is a metabolite of hormone insulin-like growth factor-1 (IGF-1). It has a cyclic structure, lipophilic nature, and is enzymatically stable which makes it a more favourable candidate for manipulating the binding-release process between IGF-1 and its binding protein, thereby normalising IGF-1 function.[16]
Synthesis and circulation[edit]
The polypeptide hormone IGF-1 is synthesized primarily in the liver upon stimulation by growth hormone (GH). It is a key mediator of anabolic activities in numerous tissues and cells, such as growth hormone-stimulated growth, metabolism and protein translation.[17] Due to its participation in the GH-IGF-1 axis it contributes among other things to the maintenance of muscle strength, muscle mass, development of the skeleton and is a key factor in brain, eye and lung development during fetal development.[18]
A deficiency of IGF-1 is associated with the increased risks of insulin resistance, glucose intolerance, diabetes type 2, as well as cardiovascular morbidity and mortality.[17][19] Studies have shown the importance of the GH-IGF-1 axis in directing development and growth, where mice with a IGF-1 deficiency had a reduced body- and tissue mass. Mice with an excessive expression of IGF-1 had an increased mass.[19]
The levels of IGF-1 in the body vary throughout life, depending on age, where peaks of the hormone is generally observed during puberty and the postnatal period. After puberty, when entering the third decade of life, there is a rapid decrease in IGF-1 levels due to the actions of GH. Between the third and eight decade of life, the IGF-1 levels decrease gradually, but unrelated to functional decline.[18] However, protein intake is proven to increase IGF-1 levels.[20]

Mechanism of action[edit]
IGF-1 is a primary mediator of the effects of growth hormone (GH). Growth hormone is made in the anterior pituitary gland, is released into the blood stream, and then stimulates the liver to produce IGF-1. IGF-1 then stimulates systemic body growth, and has growth-promoting effects on almost every cell in the body, especially skeletal muscle, cartilage, bone, liver, kidney, nerve, skin, hematopoietic, and lung cells. In addition to the insulin-like effects, IGF-1 can also regulate cellular DNA synthesis.[21]
IGF-1 binds to at least two cell surface receptor tyrosine kinases: the IGF-1 receptor (IGF1R), and the insulin receptor. Its primary action is mediated by binding to its specific receptor, IGF1R, which is present on the surface of many cell types in many tissues. Binding to the IGF1R initiates intracellular signaling. IGF-1 is one of the most potent natural activators of the AKT signaling pathway, a stimulator of cell growth and proliferation, and a potent inhibitor of programmed cell death .[22][23] The IGF-1 receptor and insuline receptor are two closely related members of a transmembrane tetrameric tyrosine kinase receptor family. They control vital brain functions, such as survival, growth, energy metabolism, longevity, neuroprotection and neuroregeneration.[24]
IGF-1 binds and activates its own receptor, IGF-1R, through the cell surface expression of Receptor Tyrosine Kinase's (RTK's), and further signals through multiple intracellular transduction cascades. IGF-1R is the critical role-playing inducer in modulating the metabolic effects of IGF-1 for cellular senescence and survival. At a localized target cell, IGF-1R elicits the mediation of paracrine activity. After its activation the initiation of intracellular signaling occurs inducing a magnitude of signaling pathways. An important mechanistic pathway involved in mediating a cascade affect regulated by phosphatidylinositol-3 kinase (PI3K) and its downstream partner, mTOR (mammalian Target of Rapamycin). Rapamycin binds with the enzyme FKBPP12 to inhibit the mTORC1 complex. mTORC2 remains unaffected and responds by up-regulating AKT, driving signals through the inhibited mTORC1. Phosphorylation of Eukaryotic translation initiation factor 4E (EIF4E) by mTOR suppresses the capacity of Eukaryotic translation initiation factor 4E-binding protein 1 (EIF4EBP1) to inhibit EIF4E and slow metabolism.[25][26] A mutation in the signaling pathway PI3K-AKT-mTOR is a big factor in the formation of tumors found predominantly on skin, internal organs, and secondary lymph nodes (Kaposi sarcoma).[26]
Metabolic effects[edit]
As a major growth factor, IGF-1 is responsible for stimulating growth of all cell types, and causing significant metabolic effects.[27] One important metabolic effect of IGF-1 is its ability to signal cells that sufficient nutrients are available for cells to undergo hypertrophy and cell division.[28] These signals also enable IGF-1 to inhibit cell apoptosis and increase the production of cellular proteins.[28] IGF-1 receptors are ubiquitous, which allows for metabolic changes caused by IGF-1 to occur in all cell types.[27] IGF-1's metabolic effects are far-reaching and can coordinate protein, carbohydrate, and fat metabolism in a variety of different cell types.[27] The regulation of IGF-1's metabolic effects on target tissues is also coordinated with other hormones such as growth hormone and insulin.[29]
Related growth factors[edit]
IGF-1 exists within the insulin/insulin-like growth factor (IGF) signaling system. The system consists of three ligands (insulin, IGF-1 and IGF-2, 2 tyrosine kinase receptors (insulin receptor and IGF-1R receptor) and six ligand binding proteins (IGFBP 1-6).[30] It plays an essential role in proliferation, survival, regulation of cell growth and affects almost every organ system in the body.[31]
Similarly to IGF-1, IGF-2 is mainly produced in the liver. After release into circulation it stimulates growth and cell proliferation. IGF-2 is thought to be a fetal growth factor, as it is essential for a normal embryonic development and is highly expressed in embryonic and neonatal tissues.[32]
A splice variant of IGF-1 sharing an identical mature region, but with a different E domain is known as mechano-growth factor (MGF).[33]
Disorders[edit]
Laron syndrome[edit]
Patients with severe primary insulin-like growth factor-1 deficiency (IGFD), called Laron syndrome (LS) or Laron dwarfism, may be treated with Mecasermin (brand name Increlex). This is a synthetic analog of IGF-1 which is approved for the treatment of growth failure.[34]
Laron syndrome does not respond at all to growth hormone treatment due to a lack of GH receptors. The FDA has grouped these diseases into a disorder called severe primary IGF deficiency. Patients with severe primary IGFD typically present with normal to high GH levels, height below 3 standard deviations (SD), and IGF-1 levels below 3 SD.[35] Severe primary IGFD includes patients with mutations in the GH receptor, post-receptor mutations or IGF mutations, as previously described. As a result, these patients cannot be expected to respond to GH treatment.[36]
People with Laron syndrome have very low rates of both cancer and diabetes.[37]
Acromegaly[edit]
Acromegaly is a syndrome that results in the anterior pituitary gland producing excess growth hormone (GH). A number of disorders may increase the pituitary's GH output, although most commonly it involves a tumor called pituitary adenoma, derived from a distinct type of cell (somatotrophs). It leads to anatomical changes and metabolic dysfunction caused by both an elevated GH and elevated IGF-1 levels.[38]
High level of IGF-1 in acromegaly is related to an increased risk of some cancers, particularly colon cancer and thyroid cancer.[39]
Use as a diagnostic test[edit]
IGF-1 levels can be analyzed and used by physicians as a screening test for growth hormone deficiency (GHD),[40] acromegaly and gigantism.[35] However, IGF-1 has been shown to be a bad diagnostic screening test for growth hormone deficiency.[41][42]
The ratio of IGF-1 and insulin-like growth factor-binding protein 3 has shown to be a useful diagnostic test for GHD.[43][44]
Causes of elevated IGF-1 levels[edit]
- acromegaly (especially when GH is also high)[38]
- high-protein diet[45]
- consumption of dairy products (except for cheese)[46]
- delayed puberty[47]
- pregnancy[48]
- hyperthyroidism[48]
- IGF-1 assay problems[48]
- some rare tumors (i.e. carcinoids) secreting IGF-1[49]
Health effects[edit]
Mortality[edit]
Both high and low levels of IGF‐1 increase mortality risk, with the mid‐range (120–160 ng/ml) being associated with the lowest mortality.[50]
Cancer[edit]
Several studies have shown associations between high levels of IGF-1 and an increased risk of tumor development. High levels of IGF-1 are associated with a 65% risk increase in the risk of premenopausal breast cancer,[51] and a 49% increase in the risk of prostate cancer.[51] One study found that with an increase in serum IGF-1 levels of 100 ng/ml, there is a corresponding 69% increase in the risk of colorectal cancer.[52][50] Another study found that high levels of IGF-1 are associated with a 106% increase in the risk of lung cancer.[53][50]
Dairy consumption[edit]
It has been suggested that consumption of IGF-1 in dairy products could increase cancer risk, particularly prostate cancer.[54][55] However, a 2018 review by the Committee on Carcinogenicity of Chemicals in Food, Consumer Products and the Environment (COC) concluded that there is "insufficient evidence to draw any firm conclusions as to whether exposure to dietary IGF-1 is associated with an increased incidence of cancer in consumers".[55] Certain dairy processes such as fermentation are known to significantly decrease IGF-1 concentrations.[56]
Cardiovascular disease[edit]
Increased IGF-1 levels are associated with a 16% lower risk of cardiovascular disease and a 28% reduction of cardiovascular events.[57]
Diabetes[edit]
Low IGF-1 levels are shown to increase the risk of developing type 2 diabetes and insulin resistance.[58] On the other hand, a high IGF-1 bioavailability in diabetes patients may delay or prevent the inception of diabetes-associated complications. A normal functioning IGF-1 mechanism reduces the occurrence of diabetes complications associated with lower IGF-1 levels, as it improves impaired small blood vessel function.[59]
IGF-1, insulin resistance, and NAFLD[edit]
The relationship between IGF-1, insulin resistance, and NAFLD is a complex interplay. On the one hand, growth hormone deficiency can lead to insulin resistance and the progression of NAFLD.[60] On the other hand, a decrease in circulating IGF-1, which can result in a chronic elevation of growth hormone levels, also contributes to insulin resistance.[61] This intricate balance makes it challenging to pinpoint the exact role of IGF-1 in hepatic insulin resistance and the development of NAFLD.
A study in which liver-deficient IGF-1 mice were treated with exogenous IGF-1 for four weeks demonstrated that IGF-1 inhibits growth hormone secretion. As a result, insulin sensitivity improved in these mice, indicating that IGF-1 is important for maintaining insulin sensitivity.[61]
In support of this, a different experiment conducted on a mouse model has demonstrated that the specific deletion of IGF-1 in the liver results in insulin resistance, indicating that hepatic IGF-1 regulates systemic insulin sensitivity. Therefore, increasing circulating IGF-1 may ameliorate NASH, at least in part, by improving insulin sensitivity.[62]
IGF-1 seems to have a distinct role in NAFLD independent of insulin resistance and growth hormone levels. For one, IGF-1 levels have been found to be reduced in individuals with NAFLD, regardless of the presence of diabetes or obesity.[63] Furthermore, a study of 55 patients with biopsy-proven NAFLD has indicated that while low levels of growth hormone are associated with hepatic steatosis, low levels of IGF-1 are more likely to be associated with a more advanced stage of NAFLD and the development of fibrosis.[64]
In concurrence with the observation that an IGF-1 deficiency may lead to liver fibrosis, IGF-1 has also been shown to abrogate fibrosis in the livers of spontaneous dwarf rats lacking growth hormone. This indicates that IGF-1 action in the liver is independent of growth hormone.[65] Moreover, the possibility of fibrosis reversion following IGF1 gene transfer into cirrhotic rat livers offers hope for its application in human health.[66] It has been suggested that while growth hormone induces lipolysis, IGF-1 is an insulin-sensitizer with possible anti-fibrotic effects.[67]
Low serum IGF-1 levels are considered a promising biomarker for predicting fibrosis, but not steatosis, in NAFLD patients.[67] A closer examination of fibrotic grade and its association with IGF-1 levels revealed that IGF-1 was significantly lower in patients with portal fibrosis (stages 1–3) than in those without portal fibrosis and was furthermore relatively low in patients showing ballooning.[64] Importantly, IGF-1 levels can be used as a biomarker for NAFLD specifically, as no changes were observed in IGF‐1 levels in patients suffering from liver fibrosis due to chronic hepatitis C.[68]
Clinical trials[edit]
Mecasermin[edit]
Mecasermin is a complex consisting of recombinant human IGF-1 and recombinant human IGF-binding protein-3.[69] The complex is used for the long-term treatment in children with growth failure, where they suffer from severe IGF-1 deficiency unresponsive to GH. Children with growth failure were given 0,12 mg/kg subcutaneous mecasermin two times a day over a period with a mean duration of 4,4 years (range: 0,04-12,5 years). During the first year of treatment the height velocity of the children increased from a mean of 2,8 cm/year at baseline to a mean of 8,0 cm/year. The mean growth velocities continued to remain above baseline for up to 8 years.[70]
Mecasermin therapy is also shown to be beneficial with other conditions including diabetes mellitus and anorexia nervosa.[70]
rhIGF-1[edit]
Several companies have evaluated administering recombinant human IGF-1 (rhIGF-1) in clinical trials for type 1 diabetes. These patients, despite having increased GH secretion, have low levels of circulating IGF-1 and therefore may benefit from rhIGF-1 therapy.[71] Results shows that a rhIGF-1 therapy two times a day in adults with type 1 diabetes increased the circulating IGF-1. This was with a reciprocal decrease in IGF-2 and an elevation of IGFBP-2.[71]
See also[edit]
References[edit]
- ^ a b c GRCh38: Ensembl release 89: ENSG00000017427 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000020053 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Tahimic CG, Wang Y, Bikle DD (2013). "Anabolic effects of IGF-1 signaling on the skeleton". Frontiers in Endocrinology. 4: 6. doi:10.3389/fendo.2013.00006. PMC 3563099. PMID 23382729.
- ^ Salmon WD, Daughaday WH (June 1957). "A hormonally controlled serum factor which stimulates sulfate incorporation by cartilage in vitro". The Journal of Laboratory and Clinical Medicine. 49 (6): 825–836. PMID 13429201.
- ^ Meuli C, Zapf J, Froesch ER (April 1978). "NSILA-carrier protein abolishes the action of nonsuppressible insulin-like activity (NSILA-S) on perfused rat heart". Diabetologia. 14 (4): 255–259. doi:10.1007/BF01219425. PMID 640301.
- ^ Höppener JW, de Pagter-Holthuizen P, Geurts van Kessel AH, Jansen M, Kittur SD, Antonarakis SE, et al. (1985). "The human gene encoding insulin-like growth factor I is located on chromosome 12". Human Genetics. 69 (2): 157–160. doi:10.1007/BF00293288. PMID 2982726. S2CID 5825276.
- ^ Jansen M, van Schaik FM, Ricker AT, Bullock B, Woods DE, Gabbay KH, et al. (1983). "Sequence of cDNA encoding human insulin-like growth factor I precursor". Nature. 306 (5943): 609–611. Bibcode:1983Natur.306..609J. doi:10.1038/306609a0. PMID 6358902. S2CID 4336584.
- ^ Rinderknecht E, Humbel RE (April 1978). "The amino acid sequence of human insulin-like growth factor I and its structural homology with proinsulin". The Journal of Biological Chemistry. 253 (8): 2769–2776. doi:10.1016/S0021-9258(17)40889-1. PMID 632300.
- ^ Callaway E (February 2022). "Big dog, little dog: mutation explains range of canine sizes". Nature. 602 (7895): 18. Bibcode:2022Natur.602...18C. doi:10.1038/d41586-022-00209-0. PMID 35087254. S2CID 246359754.
- ^ Decourtye L, Mire E, Clemessy M, Heurtier V, Ledent T, Robinson IC, et al. (2017). "IGF-1 Induces GHRH Neuronal Axon Elongation during Early Postnatal Life in Mice". PloS One. 12 (1): e0170083. Bibcode:2017PLoSO..1270083D. doi:10.1371/journal.pone.0170083. PMC 5226784. PMID 28076448.
- ^ Suwa S, Katsumata N, Maesaka H, Tokuhiro E, Yokoya S (December 1988). "Serum insulin-like growth factor I (somatomedin-C) level in normal subjects from infancy to adulthood, pituitary dwarfs and normal variant short children". Endocrinologia Japonica. 35 (6): 857–864. doi:10.1507/endocrj1954.35.857. PMID 3250861. S2CID 6965802.
- ^ Landin-Wilhelmsen K, Wilhelmsen L, Lappas G, Rosén T, Lindstedt G, Lundberg PA, et al. (September 1994). "Serum insulin-like growth factor I in a random population sample of men and women: relation to age, sex, smoking habits, coffee consumption and physical activity, blood pressure and concentrations of plasma lipids, fibrinogen, parathyroid hormone and osteocalcin". Clinical Endocrinology. 41 (3): 351–357. doi:10.1111/j.1365-2265.1994.tb02556.x. PMID 7955442. S2CID 24346368.
- ^ Keating GM (2008). "Mecasermin". BioDrugs. 22 (3): 177–188. doi:10.2165/00063030-200822030-00004. PMID 18481900.
- ^ Guan J, Li F, Kang D, Anderson T, Pitcher T, Dalrymple-Alford J, et al. (January 2023). "Cyclic Glycine-Proline (cGP) Normalises Insulin-Like Growth Factor-1 (IGF-1) Function: Clinical Significance in the Ageing Brain and in Age-Related Neurological Conditions". Molecules. 28 (3): 1021. doi:10.3390/molecules28031021. PMC 9919809. PMID 36770687.
- ^ a b Larsson SC, Michaëlsson K, Burgess S (September 2020). "IGF-1 and cardiometabolic diseases: a Mendelian randomisation study". Diabetologia. 63 (9): 1775–1782. doi:10.1007/s00125-020-05190-9. PMC 7406523. PMID 32548700.
- ^ a b Guo J, Xie J, Zhou B, Găman MA, Kord-Varkaneh H, Clark CC, et al. (1 April 2020). "The influence of zinc supplementation on IGF-1 levels in humans: A systematic review and meta-analysis". Journal of King Saud University - Science. 32 (3): 1824–1830. doi:10.1016/j.jksus.2020.01.018. ISSN 1018-3647.
- ^ a b Xie W, Tang Z, Guo Y, Zhang C, Zhang H, Han Y, et al. (September 2019). "Seasonal expressions of growth hormone receptor, insulin-like growth factor 1 and insulin-like growth factor 1 receptor in the scented glands of the muskrats (Ondatra zibethicus)". General and Comparative Endocrinology. 281: 58–66. doi:10.1016/j.ygcen.2019.05.014. PMID 31121166. S2CID 163168020.
- ^ Levine ME, Suarez JA, Brandhorst S, Balasubramanian P, Cheng CW, Madia F, et al. (March 2014). "Low protein intake is associated with a major reduction in IGF-1, cancer, and overall mortality in the 65 and younger but not older population". Cell Metabolism. 19 (3): 407–417. doi:10.1016/j.cmet.2014.02.006. PMC 3988204. PMID 24606898.
- ^ Yakar S, Rosen CJ, Beamer WG, Ackert-Bicknell CL, Wu Y, Liu JL, et al. (September 2002). "Circulating levels of IGF-1 directly regulate bone growth and density". The Journal of Clinical Investigation. 110 (6): 771–781. doi:10.1172/JCI15463. PMC 151128. PMID 12235108.
- ^ Peruzzi F, Prisco M, Dews M, Salomoni P, Grassilli E, Romano G, et al. (October 1999). "Multiple signaling pathways of the insulin-like growth factor 1 receptor in protection from apoptosis". Molecular and Cellular Biology. 19 (10): 7203–7215. doi:10.1128/mcb.19.10.7203. PMC 84713. PMID 10490655.
- ^ Juin P, Hueber AO, Littlewood T, Evan G (June 1999). "c-Myc-induced sensitization to apoptosis is mediated through cytochrome c release". Genes & Development. 13 (11): 1367–1381. doi:10.1101/gad.13.11.1367. PMC 316765. PMID 10364155.
- ^ Moloney AM, Griffin RJ, Timmons S, O'Connor R, Ravid R, O'Neill C (February 2010). "Defects in IGF-1 receptor, insulin receptor and IRS-1/2 in Alzheimer's disease indicate possible resistance to IGF-1 and insulin signalling". Neurobiology of Aging. 31 (2): 224–243. doi:10.1016/j.neurobiolaging.2008.04.002. PMID 18479783. S2CID 14265087.
- ^ Martin D, Nguyen Q, Molinolo A, Gutkind JS (May 2014). "Accumulation of dephosphorylated 4EBP after mTOR inhibition with rapamycin is sufficient to disrupt paracrine transformation by the KSHV vGPCR oncogene". Oncogene. 33 (18): 2405–2412. doi:10.1038/onc.2013.193. PMID 23708663.
- ^ a b Wang Z, Feng X, Molinolo AA, Martin D, Vitale-Cross L, Nohata N, et al. (April 2019). "4E-BP1 Is a Tumor Suppressor Protein Reactivated by mTOR Inhibition in Head and Neck Cancer". Cancer Research. 79 (7): 1438–1450. doi:10.1158/0008-5472.CAN-18-1220. PMC 6445709. PMID 30894372.
- ^ a b c Clemmons DR (June 2012). "Metabolic actions of insulin-like growth factor-I in normal physiology and diabetes". Endocrinology and Metabolism Clinics of North America. 41 (2): 425–43, vii–viii. doi:10.1016/j.ecl.2012.04.017. PMC 3374394. PMID 22682639.
- ^ a b Bikle DD, Tahimic C, Chang W, Wang Y, Philippou A, Barton ER (November 2015). "Role of IGF-I signaling in muscle bone interactions". Bone. 80: 79–88. doi:10.1016/j.bone.2015.04.036. PMC 4600536. PMID 26453498.
- ^ Clemmons DR (January 2004). "The relative roles of growth hormone and IGF-1 in controlling insulin sensitivity". The Journal of Clinical Investigation. 113 (1): 25–27. doi:10.1172/JCI200420660. PMC 300772. PMID 14702105.
- ^ García-Mato Á, Cervantes B, Murillo-Cuesta S, Rodríguez-de la Rosa L, Varela-Nieto I (September 2021). "Insulin-like Growth Factor 1 Signaling in Mammalian Hearing". Genes. 12 (10): 1553. doi:10.3390/genes12101553. PMC 8535591. PMID 34680948.
- ^ Annunziata M, Granata R, Ghigo E (March 2011). "The IGF system". Acta Diabetologica. 48 (1): 1–9. doi:10.1007/s00592-010-0227-z. PMID 21042815. S2CID 24843614.
- ^ Winston BW, Ni A, Aurora RC (2006). "Insulin-like Growth Factors". In Laurent GJ, Shapiro SD (eds.). Encyclopedia of Respiratory Medicine. pp. 339–346. doi:10.1016/B0-12-370879-6/00453-1. ISBN 978-0-12-370879-3.
GF-II appears to be essential for normal embryonic development and, as such, IGF-II is thought to be a fetal growth factor. IGF-II is highly expressed in embryonic and neonatal tissues and promotes proliferation of many cell types primarily of fetal origin.
- ^ Carpenter V, Matthews K, Devlin G, Stuart S, Jensen J, Conaglen J, et al. (February 2008). "Mechano-growth factor reduces loss of cardiac function in acute myocardial infarction". Heart, Lung & Circulation. 17 (1): 33–39. doi:10.1016/j.hlc.2007.04.013. PMID 17581790.
- ^ Rosenbloom AL (August 2007). "The role of recombinant insulin-like growth factor I in the treatment of the short child". Current Opinion in Pediatrics. 19 (4): 458–464. doi:10.1097/MOP.0b013e3282094126. PMID 17630612. S2CID 23165648.
- ^ a b Trivellin G, Daly AF, Faucz FR, Yuan B, Rostomyan L, Larco DO, et al. (December 2014). "Gigantism and acromegaly due to Xq26 microduplications and GPR101 mutation". The New England Journal of Medicine. 371 (25): 2363–2374. doi:10.1056/NEJMoa1408028. PMC 4291174. PMID 25470569.
- ^ Cohen J, Blethen S, Kuntze J, Smith SL, Lomax KG, Mathew PM (March 2014). "Managing the child with severe primary insulin-like growth factor-1 deficiency (IGFD): IGFD diagnosis and management". Drugs in R&D. 14 (1): 25–29. doi:10.1007/s40268-014-0039-7. PMC 3964293. PMID 24639006.
- ^ Guevara-Aguirre J, Balasubramanian P, Guevara-Aguirre M, Wei M, Madia F, Cheng CW, et al. (February 2011). "Growth hormone receptor deficiency is associated with a major reduction in pro-aging signaling, cancer, and diabetes in humans". Science Translational Medicine. 3 (70): 70ra13. doi:10.1126/scitranslmed.3001845. PMC 3357623. PMID 21325617.
- ^ a b Giustina A, Chanson P, Kleinberg D, Bronstein MD, Clemmons DR, Klibanski A, et al. (April 2014). "Expert consensus document: A consensus on the medical treatment of acromegaly". Nature Reviews. Endocrinology. 10 (4): 243–248. doi:10.1038/nrendo.2014.21. PMID 24566817.
- ^ AlDallal S (August 2018). "Acromegaly: a challenging condition to diagnose". review. International Journal of General Medicine. 11: 337–343. doi:10.2147/IJGM.S169611. PMC 6112775. PMID 30197531.
- ^ Shen Y, Zhang J, Zhao Y, Yan Y, Liu Y, Cai J (April 2015). "Diagnostic value of serum IGF-1 and IGFBP-3 in growth hormone deficiency: a systematic review with meta-analysis". European Journal of Pediatrics. 174 (4): 419–427. doi:10.1007/s00431-014-2406-3. PMID 25213432.
- ^ Iwayama H, Kitagawa S, Sada J, Miyamoto R, Hayakawa T, Kuroyanagi Y, et al. (August 2021). "Insulin-like growth factor-1 level is a poor diagnostic indicator of growth hormone deficiency". Scientific Reports. 11 (1): 16159. Bibcode:2021NatSR..1116159I. doi:10.1038/s41598-021-95632-0. PMC 8352887. PMID 34373538.
- ^ Fatani TH (February 2023). "Diagnostic Value of IGF-1 in Growth Hormone-Deficient Children: Is a Second Growth Hormone Stimulation Test Necessary?". Journal of the Endocrine Society. 7 (4): bvad018. doi:10.1210/jendso/bvad018. PMC 9954969. PMID 36846213.
- ^ Haj-Ahmad LM, Mahmoud MM, Sweis NW, Bsisu I, Alghrabli AM, Ibrahim AM, et al. (March 2023). "Serum IGF-1 to IGFBP-3 Molar Ratio: A Promising Diagnostic Tool for Growth Hormone Deficiency in Children". The Journal of Clinical Endocrinology and Metabolism. 108 (4): 986–994. doi:10.1210/clinem/dgac609. PMID 36251796.
- ^ Lambrecht N (March 2023). "IGF-1/IGFBP-3 Serum Ratio as a Robust Measure to Determine GH Deficiency and Guide Human Recombinant GH Therapy". The Journal of Clinical Endocrinology and Metabolism. 108 (4): e54–e55. doi:10.1210/clinem/dgac687. PMID 36454697.
- ^ Levine ME, Suarez JA, Brandhorst S, Balasubramanian P, Cheng CW, Madia F, et al. (March 2014). "Low protein intake is associated with a major reduction in IGF-1, cancer, and overall mortality in the 65 and younger but not older population". primary. Cell Metabolism. 19 (3): 407–417. doi:10.1016/j.cmet.2014.02.006. PMC 3988204. PMID 24606898.
- ^ Melnik BC, John SM, Schmitz G (June 2011). "Over-stimulation of insulin/IGF-1 signaling by western diet may promote diseases of civilization: lessons learnt from laron syndrome". primary. Nutrition & Metabolism. 8: 41. doi:10.1186/1743-7075-8-41. PMC 3141390. PMID 21699736.
- ^ Imran SA, Pelkey M, Clarke DB, Clayton D, Trainer P, Ezzat S (2010). "Spuriously Elevated Serum IGF-1 in Adult Individuals with Delayed Puberty: A Diagnostic Pitfall". primary. International Journal of Endocrinology. 2010: 1–4. doi:10.1155/2010/370692. PMC 2939391. PMID 20862389.
- ^ a b c Freda PU (August 2009). "Monitoring of acromegaly: what should be performed when GH and IGF-1 levels are discrepant?". review. Clinical Endocrinology. 71 (2): 166–170. doi:10.1111/j.1365-2265.2009.03556.x. PMC 3654652. PMID 19226264.
- ^ Phillips JD, Yeldandi A, Blum M, de Hoyos A (October 2009). "Bronchial carcinoid secreting insulin-like growth factor-1 with acromegalic features". primary. The Annals of Thoracic Surgery. 88 (4): 1350–1352. doi:10.1016/j.athoracsur.2009.02.042. PMID 19766843.
- ^ a b c Rahmani J, Montesanto A, Giovannucci E, Zand H, Barati M, Kopchick JJ, et al. (February 2022). "Association between IGF-1 levels ranges and all-cause mortality: A meta-analysis". Aging Cell. 21 (2): e13540. doi:10.1111/acel.13540. PMC 8844108. PMID 35048526.
- ^ a b Renehan AG, Zwahlen M, Minder C, O'Dwyer ST, Shalet SM, Egger M (April 2004). "Insulin-like growth factor (IGF)-I, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis". Lancet. 363 (9418): 1346–1353. doi:10.1016/S0140-6736(04)16044-3. PMID 15110491.
- ^ Ma J, Pollak MN, Giovannucci E, Chan JM, Tao Y, Hennekens CH, et al. (April 1999). "Prospective study of colorectal cancer risk in men and plasma levels of insulin-like growth factor (IGF)-I and IGF-binding protein-3". Journal of the National Cancer Institute. 91 (7): 620–625. doi:10.1093/jnci/91.7.620. PMID 10203281.
- ^ Yu H, Spitz MR, Mistry J, Gu J, Hong WK, Wu X (January 1999). "Plasma levels of insulin-like growth factor-I and lung cancer risk: a case-control analysis". Journal of the National Cancer Institute. 91 (2): 151–156. doi:10.1093/jnci/91.2.151. PMID 9923856.
- ^ Harrison S, Lennon R, Holly J, Higgins JP, Gardner M, Perks C, et al. (June 2017). "Does milk intake promote prostate cancer initiation or progression via effects on insulin-like growth factors (IGFs)? A systematic review and meta-analysis". Cancer Causes & Control. 28 (6): 497–528. doi:10.1007/s10552-017-0883-1. PMC 5400803. PMID 28361446.
- ^ a b "Statement on possible carcinogenic hazard to consumers from insulin-like growth factor-1 (IGF-1) in the diet" (PDF). assets.publishing.service.gov.uk. Retrieved 4 February 2023.
- ^ Meyer Z, Höflich C, Wirthgen E, Olm S, Hammon HM, Hoeflich A (August 2017). "Analysis of the IGF-system in milk from farm animals - Occurrence, regulation, and biomarker potential". Growth Hormone & IGF Research. 35: 1–7. doi:10.1016/j.ghir.2017.05.004. PMID 28544872.
- ^ Li T, Zhao Y, Yang X, Feng Y, Li Y, Wu Y, et al. (December 2022). "Association between insulin-like growth factor-1 and cardiovascular events: a systematic review and dose-response meta-analysis of cohort studies". Journal of Endocrinological Investigation. 45 (12): 2221–2231. doi:10.1007/s40618-022-01819-1. PMID 35596917. S2CID 248924624.
- ^ Biadgo B, Tamir W, Ambachew S (1 May 2021). "Insulin-like Growth Factor and its Therapeutic Potential for Diabetes Complications - Mechanisms and Metabolic Links: A Review". The Review of Diabetic Studies. 16 (1): 24–34. doi:10.1900/RDS.2020.16.24 (inactive 28 April 2024). PMC 9380093. PMID 33905470.
{{cite journal}}: CS1 maint: DOI inactive as of April 2024 (link) - ^ Biadgo B, Tamir W, Ambachew S (1 May 2021). "Insulin-like Growth Factor and its Therapeutic Potential for Diabetes Complications - Mechanisms and Metabolic Links: A Review". The Review of Diabetic Studies. 16 (1): 24–34. doi:10.1900/RDS.2020.16.24 (inactive 28 April 2024). PMC 9380093. PMID 33905470.
{{cite journal}}: CS1 maint: DOI inactive as of April 2024 (link) - ^ Doycheva I, Erickson D, Watt KD (September 2022). "Growth hormone deficiency and NAFLD: An overlooked and underrecognized link". Hepatology Communications. 6 (9): 2227–2237. doi:10.1002/hep4.1953. PMC 9426379. PMID 35765700.
- ^ a b Yakar S, Setser J, Zhao H, Stannard B, Haluzik M, Glatt V, et al. (January 2004). "Inhibition of growth hormone action improves insulin sensitivity in liver IGF-1-deficient mice". The Journal of Clinical Investigation. 113 (1): 96–105. doi:10.1172/JCI200417763. PMC 300761. PMID 14702113.
- ^ Yakar S, Liu JL, Fernandez AM, Wu Y, Schally AV, Frystyk J, et al. (May 2001). "Liver-specific igf-1 gene deletion leads to muscle insulin insensitivity". Diabetes. 50 (5): 1110–1118. doi:10.2337/diabetes.50.5.1110. PMID 11334415.
- ^ Arturi F, Succurro E, Procopio C, Pedace E, Mannino GC, Lugarà M, et al. (October 2011). "Nonalcoholic fatty liver disease is associated with low circulating levels of insulin-like growth factor-I". The Journal of Clinical Endocrinology and Metabolism. 96 (10): E1640–E1644. doi:10.1210/jc.2011-1227. PMID 21816784.
- ^ a b Ichikawa T, Nakao K, Hamasaki K, Furukawa R, Tsuruta S, Ueda Y, et al. (June 2007). "Role of growth hormone, insulin-like growth factor 1 and insulin-like growth factor-binding protein 3 in development of non-alcoholic fatty liver disease". Hepatology International. 1 (2): 287–294. doi:10.1007/s12072-007-9007-4. PMC 2716823. PMID 19669352.
- ^ Nishizawa H, Takahashi M, Fukuoka H, Iguchi G, Kitazawa R, Takahashi Y (June 2012). "GH-independent IGF-I action is essential to prevent the development of nonalcoholic steatohepatitis in a GH-deficient rat model". Biochemical and Biophysical Research Communications. 423 (2): 295–300. doi:10.1016/j.bbrc.2012.05.115. PMID 22659415.
- ^ Sobrevals L, Rodriguez C, Romero-Trevejo JL, Gondi G, Monreal I, Pañeda A, et al. (March 2010). "Insulin-like growth factor I gene transfer to cirrhotic liver induces fibrolysis and reduces fibrogenesis leading to cirrhosis reversion in rats". Hepatology. 51 (3): 912–921. doi:10.1002/hep.23412. PMID 20198635.
- ^ a b Dichtel LE, Corey KE, Misdraji J, Bredella MA, Schorr M, Osganian SA, et al. (January 2017). "The Association Between IGF-1 Levels and the Histologic Severity of Nonalcoholic Fatty Liver Disease". Clinical and Translational Gastroenterology. 8 (1): e217. doi:10.1038/ctg.2016.72. PMC 5288606. PMID 28125073.
- ^ Chishima S, Kogiso T, Matsushita N, Hashimoto E, Tokushige K (2017). "The Relationship between the Growth Hormone/Insulin-like Growth Factor System and the Histological Features of Nonalcoholic Fatty Liver Disease". Internal Medicine. 56 (5): 473–480. doi:10.2169/internalmedicine.56.7626. PMC 5399195. PMID 28250290.
- ^ Keegan MT (2019). "Endocrine Pharmacology". In Hemmings Jr HC, Egan TD (eds.). Pharmacology and Physiology for Anesthesia (2nd ed.). pp. 708–731. doi:10.1016/B978-0-323-48110-6.00036-3. ISBN 978-0-323-48110-6. S2CID 262107214.
Mecasermin is a complex of recombinant human IGF-1 and recombinant human IGF-binding protein-3 (rhIGFBP-3) used to treat children with severe IGF-1 deficiency unresponsive to GH.
- ^ a b Keating GM (2008). "Mecasermin". BioDrugs. 22 (3): 177–188. doi:10.2165/00063030-200822030-00004. PMID 18481900.
- ^ a b Carroll PV, Umpleby M, Alexander EL, Egel VA, Callison KV, Sönksen PH, et al. (December 1998). "Recombinant human insulin-like growth factor-I (rhIGF-I) therapy in adults with type 1 diabetes mellitus: effects on IGFs, IGF-binding proteins, glucose levels and insulin treatment". Clinical Endocrinology. 49 (6): 739–746. doi:10.1046/j.1365-2265.1998.00600.x. PMID 10209561. S2CID 20727527.
External links[edit]
- Insulin-Like+Growth+Factor+I at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Overview of all the structural information available in the PDB for UniProt: P05019 (Insulin-like growth factor I) at the PDBe-KB.

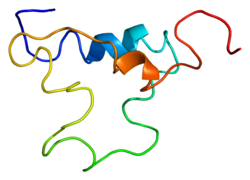

















![3lri: Solution structure and backbone dynamics of long-[Arg(3)]insulin-like growth factor-I](http://upload.wikimedia.org/wikipedia/commons/thumb/3/3b/PDB_3lri_EBI.jpg/180px-PDB_3lri_EBI.jpg)