User:Ferozemide/Bradycardia
| This is the sandbox page where you will draft your initial Wikipedia contribution.
If you're starting a new article, you can develop it here until it's ready to go live. If you're working on improvements to an existing article, copy only one section at a time of the article to this sandbox to work on, and be sure to use an edit summary linking to the article you copied from. Do not copy over the entire article. You can find additional instructions here. Remember to save your work regularly using the "Publish page" button. (It just means 'save'; it will still be in the sandbox.) You can add bold formatting to your additions to differentiate them from existing content. |
Lead[edit]
Bradycardia is a medical term used to describe a resting heart rate under 60 beats per minute (BPM) as determined by an electrocardiogram.[1] While bradycardia can result from a variety of pathologic processes, it is commonly a physiologic response to cardiovascular conditioning, or due to asymptomatic type 1 atrioventricular block. Resting heart rates less than 60 BPM are often normal during sleep in young and healthy adults, and in athletes.[2] In large population studies of adults with without underlying heart disease, 50 BPM appears to be a physiologic lower limit of normal.[3] Bradycardia is most likely to be discovered in the elderly, as both age and underlying cardiac disease progression contribute to its development.
Bradycardia may be associated with symptoms of fatigue, dyspnea, dizziness, confusion, and frank syncope due to reduced forward blood flow to the brain, lungs, and skeletal muscle.[4] The types of symptoms often depend on the etiology of the slow heart rate, classified by the anatomic location of a dysfunction within the cardiac conduction system.[5] Generally, these classifications involve the broad categories of sinus node dysfunction (SND), atrioventricular block, and other conduction tissue disease.[6] However, bradycardia can also result without dysfunction of the native conduction system, arising secondary to medications including beta blockers, calcium channel blockers, antiarrythmics, and other cholinergic drugs. Excess vagus nerve activity or carotid sinus hypersensitivity are neurological causes of transient symptomatic bradycardia. Hypothyroidism and metabolic derangements are other common extrinsic causes of bradycardia.[4]
The management of a bradycardia is generally reserved for patients with symptoms, regardless of minimum heart rate during sleep or the presence of most concomitant heart rhythm abnormalities (See: Sinus pause), which are common with this condition.[7] Untreated SND, has been shown to increase the future risk of atrial fibrillation, heart failure, and syncope, sometimes warranting definitive treatment with an implanted pacemaker.[8][9] In atrioventricular causes of bradycardia, great care is undertaken to identify reversible causes of disease.[4] However, permanent pacemaker implantation is often required when no reversible causes are found.[2] In both SND and atrioventricular blocks, there is little role for medical therapy unless a patient is hemodynamically unstable, which may require the use of medications such as atropine, isoproterenol, and interventions such as transcutaenous pacing, until such time that an appropriate workup can be undertaken and long term treatment selected.[2]
The term "relative bradycardia" can refer to a heart rate lower than that expected in a particular disease state, often a febrile illness.[10] Chronotropic incompetence (CI) refers to an inadequate rise in heart rate during periods of increased demand, often due to exercise, and is an important sign of SND and indication for pacemaker implantation.[9][2]
Athletes may have athletic heart syndrome, which includes bradycardia as part of the cardiovascular adaptations to training and participation.[11]
The word "bradycardia" is from the Greek βραδύς bradys "slow", and καρδία kardia "heart".
Normal Cardiac Conduction[edit]
A description of the normal cardiac conduction system is helpful in establishing a system of classification of the types of bradyarrythmias. The heart is a type of specialized muscle containing repeating units of cardiomyocytes, or heart muscle cells. Like most cells, cardiomyocytes maintain a highly regulated negative voltage at rest, and are capable of propagating action potentials, much like neurons.[12] While at rest, the negative cellular voltage of a cardiomyocyte can be raised above a certain threshold (so called depolarization) by an incoming action potential, causing the myocyte to contract. When these contractions occur in a coordinated fashion, the atria and ventricles of the heart will pump, delivering blood to the rest of the body.[12]
Normally, the origination of the action potential that causes cardiomyocytes to contract originates from the sinoatrial node (SA node). This collection of specialized conduction tissue is located near the superior vena cava's entrance into the right atrium.[13] The SA node contains pacemaker cells that demonstrate "automaticity" and are capable of generating regular impulses that travel through the heart and create a regular heart beat.[13]
In the beginning of the cardiac cycle, the SA node generates an electrical action potential which spreads across the right and left atria, causing the atrial contraction of the cardiac cycle.[13] This impulse carries on to the atrioventricular node (AV node), another specialized grouping of cells located in the base of the right atrium, which is the only anatomically normal electrical connection between the atria and ventricles. Impulses coursing through the AV node are slowed before carrying on to the ventricles,[14] allowing for appropriate filling of the ventricles before contraction. The SA and AV nodes are both closely regulated by fibers of the autonomic nervous system, allowing for adjustment of cardiac output by the central nervous system in times of increased metabolic demand.
Following slowed conduction through the atrioventricular node, the action potential originally produced at the SA node now flows through the His-purkinje system. The bundle of His originates in the AV and rapidly splits into a left and right branch, each destined for a different ventricle. Finally, these bundles branches terminate in the small Purkinje fibers that innervate myocardial tissue. The His-purkinje system conducts action potentials much faster than can be propagated between myocardial cells, which allows the entire ventricular myocardium to contract in a smaller length of time, improving pump function.[13]
Classification[edit]
Sinus Node[edit]
Bradycardia caused by the alterations of sinus node activity are divided into three types.
Sinus Bradycardia[edit]
Sinus bradycardia is a sinus rhythm of less than 50 BPM.[6] Cardiac action potentials are generated from the SA node, propagated through an otherwise normal conduction system, but occur at a slow rate. It is a common condition found in both healthy individuals and those considered well-conditioned athletes.[15] Studies have found that 50–85% of conditioned athletes have benign sinus bradycardia, as compared to 23% of the general population studied.[16] The heart muscle of athletes has a higher stroke volume, so requires fewer contractions to circulate the same volume of blood.[17] Asymptomatic sinus bradycardia decreases in prevalence with age. It is a common finding associated with the early hours of acute inferior myocardial infarction.
Sinus Arrhythmia[edit]
Sinus arrhythmias are heart rhythm abnormalities characterized by variations in the cardiac cycle length in excess of 120 milliseconds (longest cycle - shortest cycle).[2] These are the most common type of arrhythmia in the general population, and are usually without significant consequence. They typically occur in the young, athletes, or after administration of medications such as morphine. The types of sinus arrhythmia are separated into the respiratory and non-respiratory categories.[2]
Respiratory Sinus Arrhythmia[edit]
Respiratory Sinus Arrhythmia refers to the physiologically normal variation in heart rate due to breathing. During inspiration, vagus nerve activity decreases, reducing parasympathetic innervation of the SA node, and causing an increase in heart rate. During expiration, heart rates fall due to the converse occurring. [2]
Non-respiratory Sinus Arrhythmia[edit]
Non respiratory causes of sinus arrhythmia include sinus pause, sinus arrest, and sinoatrial exit block. Sinus pause and arrest involve slowing or arrest of automatic impulse generation from the sinus node. This can lead to asystole, or cardiac arrest, if ventricular escape rhythms do not activate to create backup sources of cardiac action potentials.[2]
Sinoatrial exit block is a similar nonrespratory phenomenon of temporarily lost SA node impulses. However, in contrast to sinus pause, the impulse is generated at the SA node, but either unable to leave or delayed from leaving the node, delaying or preventing atrial depolariziation. Therefore, the length of the pause is usually a multiple of the P-P interval as seen on electrocardiography. Like sinus pause, sinoatrial exit block can be symptomatic, especially with prolonged pauses length.
Sinus Node Dysfunction[edit]
Disease of the sinus node, referred to as sick sinus syndrome or sinus node dysfunction, covers conditions that include symptomatic sinus bradycardia or persistent chronotropic incompetence, sinoatrial block, sinus arrest, and tachycardia-bradycardia syndrome.[2] These conditions can be caused by damage to the native sinus node itself, or dysfunction of the autonomic nervous system that regulates the node, and are commonly exacerbated by medications.[2]
Atrioventricular Node[edit]
Bradycardia can also result to due to inhibition of the flow of action potentials through the atrioventricular (AV) node. While this can be normal in young patients due to intermittent, elevations in vagus nerve tone, symptomatic bradycardia due to AV node dysfunction in older people is commonly due to structural heart disease, myocardial ischemia, or age related fibrosis.[18] Notably, the AV node is capable of a degree of automaticity. In the event of loss of sinus node activity, the node can generate a backup source of cardiac impulses, albeit at a slower rate of 20-60 BPM, detailed below.[19]
Atrioventricular Block[edit]
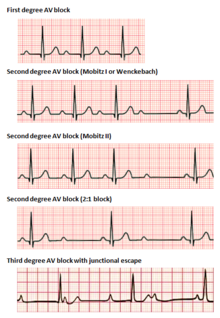
Atrioventricular (AV) blocks are divided into 3 categories, ranked by severity. AV block is diagnosed via surface ECG, which is usually sufficient to locate the causal lesion of the block, without the need of an invasive electrophysiology study.[2] There is evidence that low grade AV block lies on a spectrum of disease: 2nd degree type 1 AV block can revert to 1st degree AV block during periods of elevated sinus heart rates, and 1st degree AV blocks can progress to 2nd degree type 1 blocks during carotid sinus massage.[2]
In 1st degree AV block, electrical impulses originating in the SA node (or other ectopic focus above the ventricles) are conducted with significant delay through the AV node. This condition is diagnosed via ECG, with PR intervals in excess of 200 milliseconds.[2] The PR interval represents the length of time between the start of atrial depolarization and start of ventricular depolarization, representing the flow of electrical impulses between the SA and AV nodes. Despite the term "block", no impulses are actually fully lost in this conduction, merely delayed. The location of the causal lesion can be anywhere between the AV node and the His-Purkinje system, but is most commonly found in the AV node itself.[20] Generally, isolated PR prolongation in 1st degree AV block is not associated with increased mortality or hospitalization.[21]
2nd degree AV block is characterized by intermittently lost conduction of impulses between the SA node and the ventricles. 2nd degree block, is classified into two types. Mobitz type 1 block, otherwise known by the eponym Wenckebach, classically demonstrates grouped patterns of heart beats on ECG. Over the course of the group, the PR interval gradually lengthens, until there is a dropped conduction, resulting in no QRS complex seen on surface ECG following the last P wave. After a delay, the grouping repeats, with the PR interval shortening again to baseline.[20] Type 1 2nd degree AV block due to disease in the AV node (as opposed to in the His-purkinje system) rarely needs intervention with pacemaker implantation.[20]
2nd degree, Mobitz type 2 AV block is another phenomenon of intermittently dropped QRS complexes after characteristic groupings of beats seen on surface ECG. In this condition, the PR and RR intervals are consistent, followed by a sudden AV block and dropped QRS complex.[20] Because type 2 blocks are typically due to lesions below the AV node, the ability for ventricular escape rhythms to maintain cardiac output is compromised. Permanent pacemaker implantation is often required.[18]
Junctional Rhythm[edit]
An AV-junctional rhythm, or atrioventricular nodal bradycardia, is usually caused by the absence of the electrical impulse from the sinus node. This usually appears on an electrocardiogram (ECG) with a normal QRS complex accompanied with an inverted P wave either before, during, or after the QRS complex.[22]
An AV-junctional escape beat is a delayed heartbeat originating from an ectopic focus somewhere in the AV node. It occurs when the rate of depolarization of the SA node falls below the rate of the AV node.[22] This dysrhythmia also may occur when the electrical impulses from the SA node fail to reach the AV node because of SA or AV block.[23] This is a protective mechanism for the heart, to compensate for an SA node that is no longer handling the pacemaking activity and is one of a series of backup sites that can take over pacemaker function when the SA node fails to do so. An AV-junctional escape complex is a normal response that may result from excessive vagal tone on the SA node. Pathological causes include sinus bradycardia, sinus arrest, sinus exit block, or AV block.[22]
Ventricular[edit]
Idioventricular rhythm, also known as atrioventricular bradycardia or ventricular escape rhythm, is a heart rate of less than 50 BPM. This is a safety mechanism when a lack of electrical impulse or stimuli from the atrium occurs.[22] Impulses originating within or below the bundle of His in the AV node will produce a wide QRS complex with heart rates between 20 and 40 BPM. Those above the bundle of His, also known as junctional, will typically range between 40 and 60 BPM with a narrow QRS complex.[24][25] In a third-degree heart block, about 61% take place at the bundle branch-Purkinje system, 21% at the AV node, and 15% at the bundle of His.[25] AV block may be ruled out with an ECG indicating "a 1:1 relationship between P waves and QRS complexes."[24] Ventricular bradycardias occurs with sinus bradycardia, sinus arrest, and AV block. Treatment often consists of the administration of atropine and cardiac pacing.[22]
(atrial fibrillation, atrial flutter, and paroxysmal supraventricular tachycardia).[17]
The first, respiratory sinus arrhythmia, is usually found in young and healthy adults. Heart rate increases during inhalation and decreases during exhalation. This is thought to be caused by changes in the vagal tone during respiration.[17]
Expansion of Sinus node dysfunction
Addition of EKGs
COngenital disease
AVJ escape rhythms
Presentation[edit]
Causes[edit]
Diagnosis[edit]
Management[edit]
Epidemiology[edit]
History[edit]
Society and Culture[edit]
References[edit]
- ^ Hafeez, Yamama; Grossman, Shamai A. (2021-08-09). "Sinus bradycardia". StatPearls, NCBI Bookshelf, US National Institutes of Health. PMID 29630253. Retrieved 2022-01-16.
- ^ a b c d e f g h i j k l m Patterson, Kirsten K.; Olgin, Jeffrey E. (2022). "Bradyarrhythmias and Atrioventricular Block". Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine (12th ed.). Philadelphia, PA: Elsevier. pp. 1312–1320. ISBN 978-0-323-82467-5.
- ^ Rijnbeek, Peter R.; van Herpen, Gerard; Bots, Michiel L.; Man, Sumche; Verweij, Niek; Hofman, Albert; Hillege, Hans; Numans, Matthijs E.; Swenne, Cees A.; Witteman, Jacqueline C. M.; Kors, Jan A. (2014). "Normal values of the electrocardiogram for ages 16-90 years". Journal of Electrocardiology. 47 (6): 914–921. doi:10.1016/j.jelectrocard.2014.07.022. ISSN 1532-8430. PMID 25194872.
- ^ a b c Sidhu, Sunjeet; Marine, Joseph E. (July 2020). "Evaluating and managing bradycardia". Trends in Cardiovascular Medicine. 30 (5): 265–272. doi:10.1016/j.tcm.2019.07.001.
- ^ Patterson, Kirsten K.; Olgin, Jeffrey E. (2022). "Bradyarrhythmias and Atrioventricular Block". Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine (12th ed.). Philadelphia, PA: Elsevier. pp. 1312–1320. ISBN 978-0-323-82467-5.
- ^ a b Kusumoto, Fred M.; Schoenfeld, Mark H.; Barrett, Coletta; Edgerton, James R.; Ellenbogen, Kenneth A.; Gold, Michael R.; Goldschlager, Nora F.; Hamilton, Robert M.; Joglar, José A.; Kim, Robert J.; Lee, Richard; Marine, Joseph E.; McLeod, Christopher J.; Oken, Keith R.; Patton, Kristen K. (2019-08-20). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society". Circulation. 140 (8). doi:10.1161/CIR.0000000000000628. ISSN 0009-7322.
- ^ Sidhu, Sunjeet; Marine, Joseph E. (2020-07). "Evaluating and managing bradycardia". Trends in Cardiovascular Medicine. 30 (5): 265–272. doi:10.1016/j.tcm.2019.07.001.
{{cite journal}}: Check date values in:|date=(help) - ^ Menozzi, Carlo; Brignole, Michele; Alboni, Paolo; Boni, Luca; Paparella, Nelly; Gaggioli, Germano; Lolli, Gino (1998-11). "The natural course of untreated sick sinus syndrome and identification of the variables predictive of unfavorable outcome". The American Journal of Cardiology. 82 (10): 1205–1209. doi:10.1016/s0002-9149(98)00605-5. ISSN 0002-9149.
{{cite journal}}: Check date values in:|date=(help) - ^ a b Kusumoto, Fred M.; Schoenfeld, Mark H.; Barrett, Coletta; Edgerton, James R.; Ellenbogen, Kenneth A.; Gold, Michael R.; Goldschlager, Nora F.; Hamilton, Robert M.; Joglar, José A.; Kim, Robert J.; Lee, Richard; Marine, Joseph E.; McLeod, Christopher J.; Oken, Keith R.; Patton, Kristen K. (2019-08-20). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society". Circulation. 140 (8). doi:10.1161/CIR.0000000000000628. ISSN 0009-7322.
- ^ Ye, Fan; Hatahet, Mohamad; Youniss, Mohamed A.; Toklu, Hale Z.; Mazza, Joseph J.; Yale, Steven (2018-06). "The Clinical Significance of Relative Bradycardia". WMJ: official publication of the State Medical Society of Wisconsin. 117 (2): 73–78. ISSN 1098-1861. PMID 30048576.
{{cite journal}}: Check date values in:|date=(help) - ^ Baggish, Aaron L.; Wood, Malissa J. (2011-06-14). "Athlete's heart and cardiovascular care of the athlete: scientific and clinical update". Circulation. 123 (23): 2723–2735. doi:10.1161/CIRCULATIONAHA.110.981571. ISSN 1524-4539. PMID 21670241.
- ^ a b Loscalzo, Joseph; Keaney, John F.; MacRae, Calum A. (2022). "Basic Biology of the Cardiovascular System". Harrison's Principles of Internal Medicine (21st edition ed.). McGraw Hill.
{{cite book}}:|edition=has extra text (help) - ^ a b c d Sauer, William H.; Koplan, Bruce A.; Zei, Paul C. (2022). "Principles of Clinical Cardiac Electrophysiology". Harrison's Principles of Internal Medicine (21st edition ed.). McGraw Hill.
{{cite book}}:|edition=has extra text (help) - ^ Kurian, Thomas; Ambrosi, Christina; Hucker, William; Fedorov, Vadim V.; Efimov, Igor R. (2010-02-18). "Anatomy and Electrophysiology of the Human AV Node: FUNCTIONAL ANATOMY OF AV NODE". Pacing and Clinical Electrophysiology. 33 (6): 754–762. doi:10.1111/j.1540-8159.2010.02699.x. PMC 2889145. PMID 20180918.
{{cite journal}}: CS1 maint: PMC format (link) - ^ Hafeez, Yamama; Grossman, Shamai A. (2021-08-09). "Sinus bradycardia". StatPearls, NCBI Bookshelf, US National Institutes of Health. PMID 29630253. Retrieved 2022-01-16.
- ^ Ward, Bryan G.; Rippe, J.M. (1992). "11". Athletic Heart Syndrome. Vol. 11. Clinical Sports Medicine. pp. 259–272. doi:10.1016/S0278-5919(20)30529-9. PMID 1591784.
- ^ a b c Allan B. Wolfson, ed. (2005). Harwood-Nuss' Clinical Practice of Emergency Medicine (4th ed.). p. 260. ISBN 978-0-7817-5125-4.
- ^ a b Sauer, William H.; Koplan, Bruce A. (2022). "The Bradyarrhythmias: Disorders of the Atrioventricular Node". Harrison's Principles of Internal Medicine (21st Edition ed.). McGraw Hill.
{{cite book}}:|edition=has extra text (help) - ^ Sauer, William H.; Koplan, Bruce A. (2022). "The Bradyarrhythmias: Disorders of the Atrioventricular Node". Harrison's Principles of Internal Medicine (21st Edition ed.). McGraw Hill.
{{cite book}}:|edition=has extra text (help) - ^ a b c d Clark, Bradley A.; Prystowsky, Eric N. (2021-12). "Electrocardiography of Atrioventricular Block". Cardiac Electrophysiology Clinics. 13 (4): 599–605. doi:10.1016/j.ccep.2021.07.001.
{{cite journal}}: Check date values in:|date=(help) - ^ Aro, A. L.; Anttonen, O.; Kerola, T.; Junttila, M. J.; Tikkanen, J. T.; Rissanen, H. A.; Reunanen, A.; Huikuri, H. V. (2014-01-02). "Prognostic significance of prolonged PR interval in the general population". European Heart Journal. 35 (2): 123–129. doi:10.1093/eurheartj/eht176. ISSN 0195-668X.
- ^ a b c d e Allan B. Wolfson, ed. (2005). Harwood-Nuss' Clinical Practice of Emergency Medicine (4th ed.). p. 260. ISBN 978-0-7817-5125-4.
- ^ "AV Junctional Rhythm Disturbances (for Professionals)". American Heart Association. 4 December 2008. Retrieved 15 December 2009.
- ^ a b "Arrhythmias and Conduction Disorders". The merck Manuals: Online Medical Library. Merck Sharp and Dohme Corp. January 2008. Retrieved 16 December 2009.
- ^ a b Adams MG, Pelter MM (September 2003). "Ventricular escape rhythms". American Journal of Critical Care. 12 (5): 477–8. doi:10.4037/ajcc2003.12.5.477. PMID 14503433.
